|
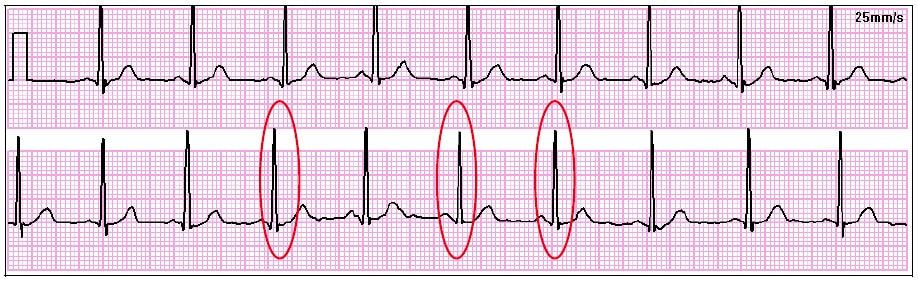
Naturopathic Medical Student Adam Sadowski back for more with this insightful post on anxiety, the autonomic nervous system and heart rate variability! With the recent passing of World Mental Day on October 10th, (which we can all agree isn’t a one day deal) and Dr. Abbott’s passion for all things meditation and mental well being, it makes sense to have a little (or lengthy) discussion about a nearly ubiquitous human experience: Anxiety, and more specifically it’s association with heart rate variability, or HRV for short. General anxiety disorder and panic disorders are some of the most common mental conditions in the United States (1,9). The difference between the two is that anxiety is mainly characterized as excessive worrying that is out of control, and panic disorder is characterized by unexpected panic attacks that can come on at any time (1,10). Unfortunately, like many mental health conditions, the medical community as a whole is not entirely sure as to what is causing this, and understandably so. The causal factor may not be so black or white, as anxiety is paired with multiple conditions creating a chicken or the egg scenario. Anxiety has been associated with but not limited to fibromyalgia3, chronic obstructive pulmonary disease (4), PTSD (5), psychosis (6), depression (7,8), borderline personality disorder (19), and cardiovascular disease (8,21). (This list could take the whole post, so we will stop there). A few interesting theories have been developed to explain these relationships such as the polyvagal theory (9), neurovisceral integration model (9), and a compromise to the central autonomic network (5). Before we discuss these theories/models, it is important to understand the role of the nervous system, and yes, it’s important to understand the intricate relationships between both anxiety and HRV to our fascinating nervous system, so buckle up… From an overly simplistic standpoint the nervous system is divided into two main branches: The Central Nervous System (commonly referred to as the CNS), and the Peripheral Nervous System (commonly referred to as the PNS). The CNS consists of the brain, brainstem, and spinal cord while the PNS consists of everything that isn’t the brain, brainstem or spinal cord. From there, the PNS can be divided into the Somatic Nervous System and the Autonomic Nervous System. The somatic nervous system is mainly involved with controlling skeletal muscles and you have more conscious regulation over it, while we have less conscious control of the Autonomic Nervous System as it is primarily involved with organ functions11 (allowing us to not think about breathing or contracting your heart 24/7). ** Note: This “automatic” regulation of breathing is not an EXCUSE to avoid becoming aware of one’s breathing and the realization that through mindful attention of one’s breathing AND conscious manipulation of such breathing, one may likely benefit in ways we will discuss later on in this post. The autonomic nervous system is further subdivided to involve 3 functions: sympathetic, parasympathetic, and enteric functions with the latter often being grouped into parasympathetic. With that being said, the sympathetic aspect can be thought of as a “fight-or-flight” response, and the parasympathetic aspect can be thought of as the “rest-and-digest” response. If the sympathetic component of the autonomic nervous system is overly activated, we get things like hyperventilation, palpitations, dizziness, tremors, chest discomfort, sweating, hot flashes, and GI distress (10). When the parasympathetic component is more active, our heart rate decreases/normalizes, we are much more relaxed, we salivate, and we are able to digest our food properly along with other functions that are not necessarily noticeable. It’s important to realize, that because the autonomic nervous system has two functions it’s trying to maintain a state of homeostasis where neither system is not excessively overriding the other (12). Again, this is not a black or white situation, and the interaction between the two systems is much more complicated than this post allows for. However, as we will see, when there is a disruption to this homeostasis, problems such as anxiety might arise. The wonderful Dr. Mike T Nelson uses the analogy of a car break and a gas pedal where “stepping on the gas” can be synonymous with sympathetic tone, and pressing on the brake is synonymous with parasympathetic tone. The harder you press on either pedals, the greater the tone respectively. Although parasympathetic sounds great, you don’t want to strictly press on the brakes because you won’t move, much like if you only press on the gas you’ll end up joy riding until you eventually crash. So as you can see, there is a sweet spot that we want to (ideally) stay in when it comes to a sympathetic or parasympathetic state. If you’re too sympathetic you’ll constantly feel stressed out, and if you’re too parasympathetic you might just want to spend all day in bed and never move. Now that we have a basic understanding of the nervous system, the first theory, the polyvagal theory, is an evolutionary model that suggests the autonomic nervous system evolved in mammals to suit their social environment via the use of the vagal nerve which is the head honcho of the autonomic nervous system. When parasympathetic function is working adequately, vagal stimulation primarily sends parasympathetic signaling allowing for slower heart rates, and better digestion. On the flip side, when vagal stimulation is overridden with sympathetic signaling, you start to feel nervous, get butterflies in your stomach, sweaty palms, and feel like your heart is going to fly out of your chest when giving a presentation to a large audience. The importance of the vagus nerve in the polyvagal theory according to Alvares et al, is in “promoting engagement, or disengagement with an individual’s social environment”9 and if someone thinks they are in a safe environment, defensive circuits of the sympathetic “fight-or-flight” are overridden by parasympathetic signals (13). Similarly, if someone perceives their environment as unsafe for whatever reason (ex. a large audience), the ability to “express positive social cues is compromised” (13). Note this can ALSO BE an entirely unconscious process of “perception”, think: air and sound pollution and even EMF; live in the city, near airports or sleep next to your Wifi?). It might be that impairment of these neural processes causes people to not know if their environment or the people they are around are safe, causing the development of anxiety (5), heighten arousal, or at least anxiety like symptoms. The neurovisceral integration model, which is similar to the polyvagal theory, suggests that the inability for the vagus nerve to inhibit sympathetic function prevents regulation of inflammatory processes, glucose regulation, and HPA axis function (13). Remember, the autonomic nervous system has nerves going to all organs and glands throughout the body, and whether they are more sympathetic or parasympathetic dominant, may determine if these organs or glands will up-regulate or down regulate the production of various substances. If there is too much sympathetic tone, this can lead to excess production/secretion of inflammatory cytokines, impaired fasting blood glucose by causing the liver to pump out glucose into the bloodstream, and a variety of other hormonal signals, which may be one explanation as to why stress is associated or possibly the cause to many chronic diseases. Lastly, the central autonomic network, (which isn’t really a theory) is a network within the brain which regulates adaptive responses to various stimuli (14). If we have a more robust nervous system that allows us to adapt to a multitude of situations, perhaps we can express a more parasympathetic state during times of non-threatening stress and thus have an experience of lessened anxiety. If you grew up in a larger family with constant arguing at the dinner table, perhaps over time your central autonomic network has been trained to create sympathetic responses to the surrounding stimuli such as multiple people in one room, the food that was being served, the yelling, etc. Now you get a little (or very) anxious when you go to parties because there are lots of people in one room, loud noises, an aversion to a specific food/food group or smell. Maybe it’s possible to train our nervous system to eventually express more parasympathetic tone during these situations over time such that we reduce our levels of anxiety in these environments. This robustness of the nervous system is what brings me to the topic of HRV. Most people know of HRV as a tool used to monitor recovery for athletes and exercise enthusiasts in response to various stress loads, however, this same tool may be beneficial for monitoring relative states of hyperarousal or anxiety. Simply put, HRV measures the R waves between heart beats (16). What do I mean by R waves? This is what I mean by R waves. In cardiology when we try to visualize the heart beating, we rely on ECG strips which can reveal to us a great deal of information about the heart in regards to how it is beating (are they normal beats? Are there arrhythmias present? Is someone suffering a heart attack? Etc.). There are 5 wave-forms that an ECG will show: “P-wave”, “Q-wave”, “R-wave”, “S-wave”, and lastly a “T-wave”. In a normal heart, this pattern almost always occurs where the first little bump is the “p-wave”, followed by a subtle downward “q-wave”, followed by the large upward rising “R-wave”. Following the R wave is the “s-wave” and we end with the last little hump of the “t-wave” before starting all over again. One of the reasons HRV is looking at the R-R intervals is because of how easily shows up on the ECG. Why do we care about these intervals? It goes back to the point I made about not wanting to be too sympathetic or too parasympathetic. If you are too dominant in one or the other, your heart rate won’t have any variability to it: For example… That flat line (indicative of no contractions) is not variable. In fact, it’s the complete opposite, it’s entirely predictable and going at a constant rate (0 beats per minute). Since there are so many interactions between neural, hormonal, and mechanical control systems both in the peripheral and central nervous system, a normal resting rhythm is not exactly monotonous (15). What is preferred to be seen is something like this: Granted, we don’t want to see so much variability that it looks entirely erratic and emergency medical interventions need to be used, it is very small millisecond differences between intervals that are sought after (i.e. 1.68 milliseconds at one interval and 1.66 milliseconds at the second interval followed by 1.7 milliseconds at the third, etc.) HRV can further be measured in 3 different ways, and they don’t require an ECG machine and a host of electrodes to hook yourself up to. There are smart-phone apps such as heart math and ithlete that can hook up to a variety of devices such as a polar monitor strap depending on the program. The first way HRV can be measured is through a time domain, the second way is through a frequency domain, and lastly, it can be measured through what is referred to as a non-linear domain. Time Domain looks at multiple R-to-R intervals over time (so how much time takes place between each wave). If there is more variability, the time between waves will be slightly longer or shorter. This also means your heart rate is slower and more indicative of a parasympathetic state. When vagal parasympathetic tone is in a “sweet-spot” the variability from one R wave to the next increases which can be used as a marker for health and recovery of the autonomic nervous system. It’s a good way to get an overall representation of HRV status (17). In some studies, those with anxiety have shorter time domain HRV compared to “healthy” controls, however, this findings may also be skewed by relative publication bias (5). Frequency Domain is useful when looking at how different one wav form is from another (so quite literally, the beat to beat difference). The main components that seem to be represented in the literature from frequency domain are the high frequency (largely parasympathetic influence), low frequency (largely sympathetic influence), very low frequency (a mix of the two, although there seems to be disagreement with researchers in it’s use [5]), and the low frequency to high frequency ratio. Non-linear Domain is more complicated to explain and is more important with regards to collecting data, and from what I have read in the literature thus far, is not reported as much as frequency or time domain. Regardless of the method used to obtain data, HRV is done for anywhere from 2 minutes to 24 hours (5). So what does all this HRV stuff mean when it comes to anxiety? It seems to be, that across the board those with anxiety have a decreased heart rate variability (8,16,18,20,22), indicating a more stressful state (which also makes sense as anxiety can often be a comorbidity of stress and vice-versa). Those with general anxiety disorder and social anxiety disorder have a decrease in high frequency HRV (5), and interestingly people with anxiety do not have much of a difference in low frequency HRV compared to “normal” people although there seems to be quite a bit of heterogeneity across studies which might explain this5. I do want to make a disclaimer in that, almost all of these studies I have referenced had pretty low numbers of participants and much of this information is a correlation not necessarily a causation. We do not know EXACTLY why people who have anxiety have lower HRV compared to people who do not, however, there are still some interesting reasons that were discussed above that may cause us to think about sympathetic and parasympathetic regulation as a factor. If we follow the model that those with anxiety tend to have depressed HRV and higher levels of stress, reducing stress and increasing HRV theoretically could be used to improve, or dare I say, cure one’s anxiety. The benefit of using HRV is that it will give you a quantitative measure to help monitor your stress each day. If the HRV is going up, your body may be coping better with stressors and can help to see if what you are doing is helping to alleviate your anxiety. By having that quantitative data, it may help to encourage you to keep doing whatever it is you are doing or what may need to be improved. Perhaps increasing HRV can be possible through pharmaceutical agents, practices such as yoga or meditation, exercising properly, play (whatever that means to you), adequate sleep, nutrition and/or supplementation. These are things that need to be investigated further and will be addressed in a future post. Regardless of the cause or treatment, it needs to be dealt with as it is currently costing the world one TRILLION dollars annually, (2) and it is projected to increase to six trillion by 2030 (9). 1. Locke A., Kirst N., Shultz C. Diagnosis and management of generalized anxiety disorder and panic disorder in adults. Am Fam Physician. 2015 May 1;91(9).
2. http://www.who.int/mediacentre/news/releases/2016/depression-anxiety-treatment/en/ 3. Bilgin S, Arslan E, Elmas O, et al. Investigation of the relationship between anxiety and heart rate variability in fibromyalgia: A new quantitative approach to evaluate anxiety level in fibromyalgia syndrome. Comput Biol Med. 2015;67:126-35. 4. Suh S, Ellis RJ, Sollers JJ, Thayer JF, Yang HC, Emery CF. The effect of anxiety on heart rate variability, depression, and sleep in chronic obstructive pulmonary disease. J Psychosom Res. 2013;74(5):407-13. 5. Chalmers JA, Quintana DS, Abbott MJ, Kemp AH. Anxiety Disorders are Associated with Reduced Heart Rate Variability: A Meta-Analysis. Front Psychiatry. 2014;5:80. 6. Mcausland L, Addington J. Biofeedback to treat anxiety in young people at clinical high risk for developing psychosis. Early Interv Psychiatry. 2016; 7. Paniccia M, Paniccia D, Thomas S, Taha T, Reed N. Clinical and non-clinical depression and anxiety in young people: A scoping review on heart rate variability. Auton Neurosci. 2017; 8. Chalmers JA, Heathers JA, Abbott MJ, Kemp AH, Quintana DS. Worry is associated with robust reductions in heart rate variability: a transdiagnostic study of anxiety psychopathology. BMC Psychol. 2016;4(1):32 9. Alvares GA, Quintana DS, Kemp AH, et al. Reduced heart rate variability in social anxiety disorder: associations with gender and symptom severity. PLoS ONE. 2013;8(7):e70468. 10. Diveky T, Prasko J, Kamaradova D, et al. Comparison of heart rate variability in patients with panic disorder during cognitive behavioral therapy program. Psychiatr Danub. 2013;25(1):62-7. 11. Wehrwein EA, Orer HS, Barman SM. Overview of the Anatomy, Physiology, and Pharmacology of the Autonomic Nervous System. Compr Physiol. 2016;6(3):1239-78. 12. OpenStax, Anatomy & Physiology. OpenStax. 25 April 2013. <http://cnx.org/content/col11496/latest/>. 13. Kemp AH, Quintana DS. The relationship between mental and physical health: insights from the study of heart rate variability. Int J Psychophysiol. 2013;89(3):288-96. 14. Penzlin AI, Barlinn K, Illigens BM, Weidner K, Siepmann M, Siepmann T. Effect of short-term heart rate variability biofeedback on long-term abstinence in alcohol dependent patients - a one-year follow-up. BMC Psychiatry. 2017;17(1):325. 15. Shaffer F, Mccraty R, Zerr CL. A healthy heart is not a metronome: an integrative review of the heart's anatomy and heart rate variability. Front Psychol. 2014;5:1040. 16. Goessl VC, Curtiss JE, Hofmann SG. The effect of heart rate variability biofeedback training on stress and anxiety: a meta-analysis. Psychol Med. 2017;47(15):2578-2586. 17. https://www.datasci.com/solutions/cardiovascular/heart-rate-variability 18. Fleet R, Lavoie K, Beitman BD. Is panic disorder associated with coronary artery disease? A critical review of the literature. J Psychosom Res. 2000;48(4-5):347-56. 19. Koenig J, Kemp AH, Feeling NR, Thayer JF, Kaess M. Resting state vagal tone in borderline personality disorder: A meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2016;64:18-26. 20. Levine JC, Fleming R, Piedmont JI, Cain SM, Chen WJ. Heart rate variability and generalized anxiety disorder during laboratory-induced worry and aversive imagery. J Affect Disord. 2016;205:207-215. 21. Machado S, Sancassiani F, Paes F, Rocha N, Murillo-rodriguez E, Nardi AE. Panic disorder and cardiovascular diseases: an overview. Int Rev Psychiatry. 2017;29(5):436-444. 22. Paniccia M, Paniccia D, Thomas S, Taha T, Reed N. Clinical and non-clinical depression and anxiety in young people: A scoping review on heart rate variability. Auton Neurosci. 2017;
1 Comment
Compassion Fatigue: Does It Really Exist? An interesting question and one that will not have a straightforward or short answer. As part of my exposure to reflective and self care practices through the University of Virginia School of Nursing and the Compassionate Care Initiative, I have been beyond blessed to meet some of the leaders and pioneers seeking to reverse this supposed “compassion fatigue” and more importantly, optimize one’s capacity to be fully present with another’s suffering AND feel competent and empowered to act courageously for its relief. As I have shared before in a previous post, I have used the reflective mantra/positive affirmation below to provide me with strength in the most challenging moments to remain competent and empathetic when faced with serious suffering. May I remain open to the heart, so that I may be fully for its relief May there be peace for those who seek it We are our own strength Repeating this every morning and simply when the moment called for its reflective recitation, I have gained strength and assurance in my work as a clinician and healer, but more importantly as a caring human being. Just yesterday, while driving back from my home in Charlottesville to my residency program in Winchester, I was blessed to hear a podcast between two of the most compassionate souls on this planet, Krista Tippett and Roshi Joan Halifax. As I alluded to in the introduction, I have been beyond fortunate to have met and practiced with Roshi Joan Halifax (hoping my path will someday cross with Krista), and have been moved tremendously every time I’ve heard her soothing and engaged voice. I encourage you, if you find time in your day, to listen to their conversation. Buoyancy Rather than Burnout https://onbeing.org/programs/joan-halifax-buoyancy-rather-than-burnout-in-our-lives-oct2017/ Your heart will be glad that you did. Now it would be silly of me to try to come up with anything more profound than what was said in this conversation, but I do want to highlight two fundamental ideas discussed in the podcast. The first is the idea of the great deceiver to compassion: Pity Thupten Jinpa has often called this the great imitator of compassion, an unfortunate, subtle and insidious emotion that allows one to create a barrier from another's hurt, elevating your being from the state of suffering as to protect your heart from the flames. One of my dear friends, Jonathan Bartels shares quite eloquently the idea that as caregivers you will walk into the burning fires of people's lives and through the rainstorms of another's pain, so why would you not expect to get burned? to get wet? Umbrellas and firesuits seem like great solutions to this problem, but unfortunately, they are simply the wardrobe of pity, not compassion. (Fun side note: For the biblical scholars, does Daniel and the furnace ring any bells?) When you enter the fires and rainstorms with compassion, you will be burned, you will feel the rain falling, but you will realize that you are not the rain, you are not the fire and that indeed you actually do not need armor or a raincoat to protect yourself during the storm, you just need a change of clothes once you get out. A change of clothes? Yes A change of clothes And what exactly do I mean when I say a change of clothes? Reflective, contemplative, and self care practices Pausing to breath, stopping to meditate, stepping into nature, taking a minute to pray, washing your hands after leaving the room and saying I am whole, I am here, I simply am. That is your change of clothes, that is your wardrobe, that is compassion. And the second and final idea is one that may be controversial, may be difficult to understand and is certainly challenging to practice, but an idea nonetheless that I think is important to discuss. In a time when hurt is constantly thrust into our lives from incessantly updated media, we are often sucked into the empathetic, hurting vortex of pain created from suffering thousands of miles away. I will be honest and tell you that I do not watch TV, I do not stay up to date with most public events. I am not regularly reading the paper and I can't remember the last time I sat down to watch anything on a news program. It is my choice. Am I an uninformed, ignorant and careless soul living under a rock? To some, perhaps. But in my eyes I see things a little differently. To be fair, I have experimented with the practice of engaging or disengaging from regular news outlets and have come to realize that if I let the images of popular media into my life, my heart is often overwhelmed, distracted and confused on where and how to beat to stop the flames of hurt present in my life. I have come to realize, you see, that in order to remain open to the hurt present in my life and fully for its relief, I cannot simultaneously extend my gaze to the hurt into which I cannot physically walk AND the hurt sitting right in front of my eyes. The images of hurt on TV? on social media? They are torches thrown into your life, shrapnel, the debris of suffering. They are not the fires in front of your feet. They are not the storm clouds forming above your head. Yes, they are fires, fires in need of tending, of gentle extinguishing, but not the fires on your door step. As a clinician I am surrounded my storms and fires into which I can PHYSICALLY walk, dance and pray, and I believe without a shred of doubt that my PURPOSE is to walk, dance and pray in THESE storms, not to catch the grenades thrown from the outside or to huddle with the flames burning from afar. With the practices of self care, purposeful refection and daily contemplation, I have and will continue to find the faith to walk into MY STORMS, MY FIRES, MY BURNING CHAOS. Without distraction, without deterrence, without fear. What would the world look like if we all fixed our gaze and dedicated our efforts to step into the storms and fires burning on our very door steps? I don't know about you, but that sounds like a recipe for covering the globe in compassion if you ask me. We may think we can hug the globe, but in reality, we will only cover the globe with love by stretching our hearts and finding the hand of our neighbor knowing in faith, that our other hand, and theirs, will not be empty. Shrink your gaze, expand your heart, and stop every day to change your clothes. It is time for suffering to meet its maker. GUEST POST: CHLOE FRANCIS When Rob asked me to write, from miles away over skype, I had a weird idea. We’re after insights you see – and what on earth do I have a unique insight on? Solar Panels (my job)? Britain (my home)? German language (my interest)? Actually, the theme I landed on, the thing I really wanted to write about, was definitions. So thank you Rob for the chance to do some thinking and some writing, and here’s a few musings on the power of a definition. During my first week at secondary school (named middle school in the US, I believe) I let a new friend drag me along to a lunchtime club called “writers club.” I’m not sure why, as at that time there were a thousand things I would rather do with my lunchtime than pen poetry, but I was 11 years old and needed friends, so off we went to writers club. Across the splintering wooden desks (this was in the days before they painted them all purple…) appeared an English language teacher whom I soon learnt to be both kind and severe – but most importantly for our story, she had a bit of a creative streak. I believe it was that very same creative streak that led her to set us the following homework a few years later: write a list of words that define you. Writing a list is easy, I thought – what a great task! My list looked something like this:
The only word I might add to it today would be graduate. As with many good lessons, I only managed to chase down the complexity of what I’d learnt a while later… How can I be defined in a list? I’m not sure I can even be defined by words so a list definitely won’t do. Surely I’m more defined by my actions than my words? Can I even define myself or do I need a less biased outside force to do it for me? My self-image isn’t going to be the same as my unwarped, plain self after all, right? At which point does one of my characteristics or interests qualify as something that defines me? I’ve put dancer on the list, but not skier. Why? Does the order matter? Why have I put friend before my family-based definitions like daughter and sister? (I personally don’t think the order matters, no) Why am I even doing all this defining anyway? Why do we define things? That last question, at least, I decided I could answer. I’m a scientist, and in science we really like definitions. For example, if I wanted to look at the properties of a gas (its pressure, volume etc.), the very first thing I would do is define that gas. What are its molecules like (hard spheres maybe?) and if it were in a closed container would its molecules bounce off the walls or would they transfer energy as they collide with the walls? Only once we’ve got all the definitions of the gas sorted can we use some maths to look at its properties, not before. Throughout my degree, if I was braindead before an exam I would focus on learning the definitions – they contained so much of the important information that would be needed in the exam hall. In science, definitions are more than helpful, they’re necessary and we use them to make a framework within which we can carry out scientific enquiry. Whether they’re necessary outside of areas like science though? I’m not too sure. Their power in science is so helpful, their power elsewhere could be misused. My example for this comes from a kayaking trip along a river. In Cambridge (UK) it’s not entirely unusual to find yourself in a kayak or a punt on the river. It’s even less unusual to find yourself entering into discussions…it is a university town after all. This time we were discussing race and sexuality, but more specifically my newly formed opinion that neither need be defined. Reading about the recent riots in Charlottesville, what shocked me (beyond the obvious) was actually how people still voluntarily define themselves by the colour of their skin. I wouldn’t say that I’m white – they’re just not words that I ever need say! It’s not something that defines me. I’m a friend, a daughter, a sister, a dancer, an optimist, a traveller, a scientist, a linguist, a graduate and I happen to have white skin – but that’s a descriptor, not a definition. The same applies to sexuality – if we take away the need to declare (aka define ourselves by) a sexuality it removes the power that definition has. For medical forms, sure, for everyday life – not required! So much prejudice is based on things that people have declared themselves to be or society has defined them as. If we can loosen the power of those definitions can we also shake off the prejudice? I can’t claim to know the answer to that one. I would like to think I’m right, but I don’t want to say we should loosen up the definitions at the expense of talking about these things at all. I think the key thing is to know how much we influence our own experiences with the vocabulary we use. This became obvious as an exchange student in Germany – there are simply some German words that capture an experience that English words can’t. Fernweh for example, which means the opposite of homesickness (it’s the longing for foreign lands and adventure!), is something I’ve experienced much more since I’ve had a word to assign to that feeling. Going back to our initial examples, saying “I’m white” carries more power that saying “I have white skin.” Saying “I’m straight” is a definition, saying “I’m attracted to the opposite sex” is not. So I did end up writing about German language after all! It’s unavoidable really. Doing the thinking behind this piece has brought up more questions than I’ve been able to answer, but that’s what all good discussion topics do right? As the graduate, linguist, scientist, traveller, optimist, dancer, sister, daughter, friend……and writer, that I am, I will sign off here and say thank you for reading, I hope it has given just a little food for thought Chloe Francis is a research scientist in the field of solar technologies in Cambridge, UK. She is a graduate of the University of York (UK) with a master’s degree in Chemistry. Outside of the lab she’s a keen dancer and traveller, in fact this is the first time she’s ever attempted to blog about something other than travel!
|
The MessageDedicated to the flourishing of your being Archives
November 2018
Categories |








 RSS Feed
RSS Feed